What Is Duodenal Atresia?
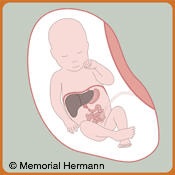 The duodenum is the first portion of small intestine after the stomach that has many connections to and shares blood vessels with other organs such as the liver, gallbladder, and pancreas. When part of the bowel fails to develop normally in the fetus, a blockage of the duodenum can occur, otherwise known as an atresia or bowel obstruction. Duodenal atresias can occur as a complete or partial blockage of any portion of the duodenum. Newborns diagnosed with duodenal atresia often present with vomiting.
The duodenum is the first portion of small intestine after the stomach that has many connections to and shares blood vessels with other organs such as the liver, gallbladder, and pancreas. When part of the bowel fails to develop normally in the fetus, a blockage of the duodenum can occur, otherwise known as an atresia or bowel obstruction. Duodenal atresias can occur as a complete or partial blockage of any portion of the duodenum. Newborns diagnosed with duodenal atresia often present with vomiting.
Duodenal atresia occurs between 1 in 1,000 and 1 in 5,000 live births. About 1/3 of infants born with duodenal atresia will also have Down Syndrome. Because of this association, newborns are often tested for other problems such a heart defects.
What Will Happen During Pregnancy?
In general, duodenal atresia is difficult to diagnose during pregnancy. Prenatal diagnosis is usually based on non-specific signs on fetal ultrasound such as a dilated stomach. Because the amniotic fluid is normally swallowed and digested by the fetus, duodenal atresia can cause an increase in fluid in the amniotic sac, hydramnios. Although there are many other causes of hydramnios, this may be a first sign of a duodenal atresia.
Duodenal atresia may be suspected by a routine prenatal ultrasound in the third trimester. Although the ultrasound may be suggestive that there is an abnormality, it cannot determine with 100% certainty that there is a bowel obstruction.
The obstetrician may order a special ultrasound that will examine the baby's heart, also known as a fetal echocardiogram, and recommend an amniocentesis to look for chromosomal abnormalities. The mother's amniotic fluid and the growth of the baby will be monitored closely with ultrasound by the obstetrician. Severe hydramnios may put the mother at risk for early delivery.
The fetal team will closely evaluate your fetus with duodenal atresia and help determine the best course of treatment. Your pregnancy will be closely monitored for complications. The Center coordinator will keep you in contact with the appropriate physicians and specialists as well as coordinating the care for you and your baby after delivery.
Will a Fetal Treatment Be Required?
Although there are no prenatal treatment options for a baby with duodenal atresia, careful planning of delivery and care of the baby after birth can make a smooth transition for mother and child.
What Special Considerations Should Be Made for Delivery?
Type of delivery: Babies with duodenal atresia usually do not need a cesarean delivery. The delivery plan will be discussed with you and your obstetrician.
Place of delivery: As long as the baby does not demonstrate signs of distress, he or she can be cared for and delivered with usual obstetrical precautions. After birth, the baby can be safely transported to a treatment center with doctors and services such as a neonatal intensive care unit and pediatric surgery. A child diagnosed with duodenal atresia will require an operation to address the problem and may stay in the hospital for several weeks.
Time of delivery:Intentional early delivery does not improve outcome. However, increasing amniotic fluid levels (hydramnios) does raise the chance for preterm delivery. If complications arise, the obstetrician may decide to induce delivery earlier than the expected due date.
 What Will Happen at Birth?
What Will Happen at Birth?
In most cases, a child with duodenal atresia will be born without any immediate problems. Afterwards, he or she will be taken to the neonatal intensive care unit. The neonatologists, specialized doctors for high risk babies, will immediately assess your baby and begin appropriate treatment, if necessary. In most cases, you and your family will be able to see and hold your newborn.
What Will Happen After Delivery?
Once the baby has been fully assessed, a pediatric surgeon will evaluate your newborn. Additional tests may be required to confirm a suspected diagnosis of duodenal atresia. Newborns with duodenal atresia will need an operation in order to fix the intestinal atresia. The goal of this surgery is to remove the bowel obstruction and allow the digestive tract to be functional.
Your surgeon will wait until there are signs of good bowel function before starting to feed the baby. Bowel function may occur in days to weeks. On average, it takes approximately two to three weeks before the intestinal tract functions fully.
Meanwhile, nutrition through a vein will be provided to the baby. The baby will receive all of the calories necessary to grow until he or she can be fed through the intestinal tract. Once bowel function returns, it will take a period of time before he or she can handle enough formula or breast milk to provide full nutrition.
The baby is likely to stay in the hospital for several weeks. Sometimes this can be much longer, depending on the degree of prematurity and the condition of the bowel.
What Are the Long-Term Outcomes and Considerations?
The potential immediate complications after surgery include leaking from the repaired bowel connections, bleeding, and infection inside the abdomen and wound. The severity and treatment of these complications should be discussed with your pediatric surgeon if they occur. The overall outcomes for most duodenal atresias are excellent depending on the presence of additional problems. Most infants may have minor intestinal problems in the first few weeks, but will recover and lead completely normal lives.
The Center team will help care for you and your infant with duodenal atresia. The Center will develop a comprehensive plan with all of the physicians and specialists involved in the care of you and your newborn before, during, and after delivery.
Contact Us
When you contact The Fetal Center, you will be in touch with a dedicated coordinator who will walk you through the process step-by-step and help you to understand every aspect of your care.
The Fetal Center at Children's Memorial Hermann Hospital
UT Professional Building
6410 Fannin, Suite 210
Houston, Texas 77030
Phone: (832) 325-7288
Toll free: (888) 818-4818
Fax: (713) 383-1464
Email: thefetalcenter@memorialhermann.org
To contact The Fetal Center at Children's Memorial Hermann Hospital, please fill out the form below.
If you are experiencing a medical emergency, call 911 or go to the nearest emergency room.
If you or someone you know needs support from the Suicide and Crisis Lifeline, call or text 988.
Located within the Texas Medical Center, The Fetal Center is affiliated with McGovern Medical School at UTHealth Houston, UT Physicians and Children’s Memorial Hermann Hospital.