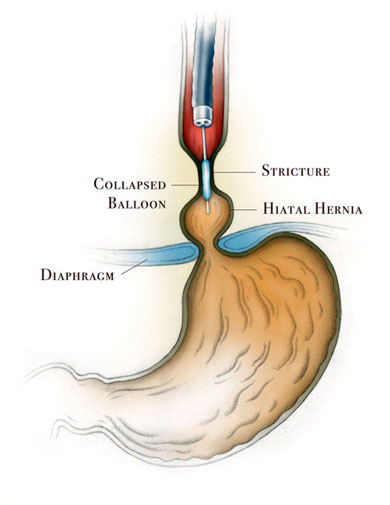
A peptic esophageal stricture (narrowing of the esophageal lumen) is one of the late complications of gastroesophageal reflux disease and occurs in 1% to 5% of patients who develop esophagitis (irritation and inflammation of the lining of the esophagus). It is one of the most difficult complications of gastroesophageal disease to manage.
What Are the Causes of Peptic Esophageal Stricture?
Peptic esophageal stricture is caused by severe gastroesophageal reflux disease and continuous damage of the lining of the esophagus by the stomach acid refluxing into the esophagus, resulting in scar and narrowing of the lumen of the esophagus.
What Are the Symptoms of Peptic Esophageal Stricture?
Patients may present with both typical (common) and atypical (uncommon) symptoms of reflux, but dysphagia (difficulty swallowing) and regurgitation of food after eating are the main symptoms.
Common Symptoms
- Heartburn (a burning sensation behind the breast bone)
- Dysphagia (difficulty swallowing or the sensation that food is hanging up or not passing down into the stomach properly)
- Regurgitation of food or liquids after eating
Uncommon Symptoms
- Chest pain
- Hoarseness
- Cough
- Pneumonia
How Is Peptic Esophageal Stricture Treated?
Many patients succeed in relieving most if not all the symptoms of GERD by making lifestyle and diet changes. Other patients require medications to control symptoms.
Other procedures used to treat peptic esophageal stricture include:
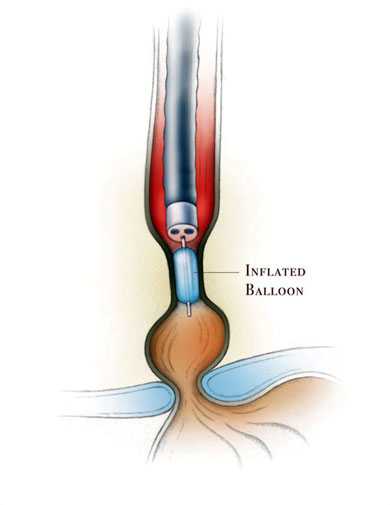
Dilation
The stricture can be dilated by using esophageal dilators, using bougies (plastic tubes that are passed from the mouth into the esophagus to dilate the esophagus) or balloon dilators during an upper endoscopy. The procedure may need to be repeated multiple times. The complete control of gastroesophageal reflux will help healing of the stricture. Aggressive acid suppression therapy with proton pump inhibitors has reduced the incidence of strictures. Despite this advance in therapy, 30% of patients with strictures require a repeat dilation within one year.
Esophageal Stenting
Esophageal stents are a relatively safe and effective method of palliation (improvement of symptoms) and treatment of peptic esophageal strictures.
Surgical Treatment
In patients who do not respond to medications and multiple esophageal dilation, surgery should be considered. The most efficient method of treating a reflux stricture has been dilation followed by an antireflux procedure to obtain complete control of gastroesophageal reflux. The aim of the surgical treatment is to restore the function of the lower esophageal sphincter (the valve between the esophagus and the stomach), to prevent the reflux of acid and bile (non-acidic juice) from the stomach into the esophagus and help healing of the stricture. The most common procedure to restore the function of the lower esophageal sphincter and prevent the gastroesophageal reflux is a minimally invasive procedure called laparoscopic Nissen fundoplication.
Strictures associated with severe esophageal dysmotility (non functional esophagus) are extremely difficult to manage. In some extreme cases, esophagectomy (esophageal replacement) may be needed.
Contact Us
If you have questions or are looking for more information, please complete the form below and we will contact you.